Lung cancer is one of the most dangerous types of cancer, being among those with the highest incidence and mortality rates in the world. Although great advances have been made in its treatment-particularly in cases where targeted therapies are applied-the challenge of recurrence has always stood in the way of progress. A new study has unraveled important mechanisms that explain why lung cancer recurs, even after apparently successful treatment. The finding could hold the key to preventing recurrence and greatly improving survival rates for patients with this aggressive disease.
The Fight Against Lung Cancer: A Two-Front Battle
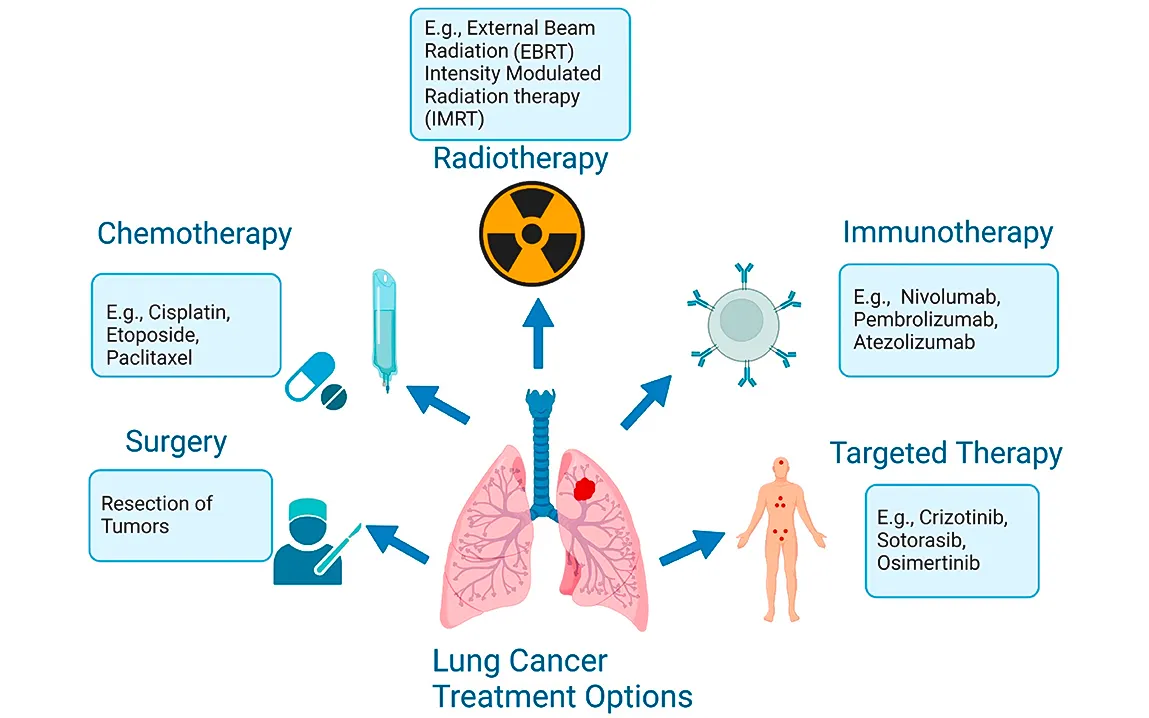
Targeted therapies have become a cornerstone in the treatment of NSCLC, especially for patients with EGFR mutations over the recent years. These targeted therapies, such as osimertinib, have shown their promise by effectively halting tumor growth and extending survival. However, one of the most persistent challenges in the field is the phenomenon of drug resistance, where cancer cells, once susceptible to treatment, adapt and begin to evade the effects of the drugs.
The new study puts light on the detailed mechanism that allows these drug-resistant cells to not only survive but thrive and eventually lead to cancer recurrence. It is here-in this niche, that is, within the immediate vicinity around a tumor, termed the tumor microenvironment-that has become a source for the discovery of an important actor in such resistance. The tumor microenvironment encompasses various types of cells, extracellular components, and signaling pathways bi-directionally interacting with the tumor cells while affecting the behaviors implicated in poorer approaches to treatments.
Tumor Microenvironment: The Battlefield
Far from being a passive bystander, the tumor microenvironment actively fosters a milieu in which the various resistance mechanisms will further make sure that recurring lung cancer becomes such a formidable opponent. For example, the immune-suppressive cell subpopulations in the TME have effects on lowering the immunity of the body against cancer, hence building a protective sheath around the tumor cells. Moreover, some of the molecules within the TME promote the survival of cancer cells in unfavorable conditions, which allows them to evade therapies and grow uncontrollably.
In lung cancer, particularly those with EGFR mutations, this microenvironment is altered dramatically after the first treatment. Residual cancer cells that survived the drug treatment often changed character to help them avoid further attacks, the study said. These cells are not necessarily immune to the drugs but have developed a form of tolerance that allows them to persist in a dormant state, only to proliferate later, causing the cancer to return more aggressively.
Unveiling the Molecular Pathways Driving Recurrence
Key findings in the present study decipher molecular pathways, enabling these tumor cells to bypass or resist drug therapy. A variety of signaling has been identified, represented as the S100A9-ALDH1A1-RA axis, and apparently drives recurrence subsequent to drug therapy. This is a crucial path for the post-treatment survival of drug tolerance, hidden away in the TME.
In one of those “Aha!” moments, they hit upon a pathway in preclinical models that showed interference with the S100A9-ALDH1A1-RA signaling pathway to prevent cancer recurrence. This opens a window of opportunity in the development of new treatments specifically targeting these “drug-tolerant” cells and prevents them from going into “hiding” to emerge in the future as lethal cancer.
The Role of Drug Combinations in Overcoming Resistance
It also points to the possibility of using combination therapies to overcome resistance. Combining existing targeted therapies with drugs that can block the key pathways involved in recurrence, it is possible to prevent the cancer from returning, believe the researchers. Using a combination of osimertinib, a drug already in clinical use, with new inhibitors targeting the S100A9-ALDH1A1-RA pathway, showed promising results in animal models. These findings suggest that the treatment of lung cancer has to be done in a more person-specific manner since the tumor environment is dynamic; this could extend the period of time when patients are in remission considerably.
Moreover, the research emphasizes how TME monitoring should be conducted without interruption, alongside the molecular pathways of drug resistance. The evolutionary understanding of the latter will hold the key for future strategies aimed at preventing resistance well before it gains ground.
Implications for Future Treatments
This thus represents a massive leap forward in the complexity of drug resistance in lung cancer. While providing insight not only into molecular and environmental contributors to recurrence, this work also opens the door to innovative treatment strategies. Findings offer hope for patients who might otherwise face recurrence of their disease and offer the possibility of longer survival and better quality of life.
The possibility of targeting the drug-tolerant cells specifically instead of relying only on traditional therapies may revolutionize the treatment of lung cancer. By focusing on the tumor microenvironment, there is growing appreciation that cancer is not a disease of rogue cells but a disease deeply intertwined with the body’s systems and responses. The interaction between the tumour cells and the immune system and the TME may prove to be a key player in cancer research in the future years to come.
Conclusion: New Horizon in Lung Cancer Treatment
Although lung cancer remains one of the most lethal forms of cancer globally, this new understanding of drug resistance brings in a glimmer of hope. Identification of mechanisms allowing cancer cells to evade initial therapies and relapse was a critical discovery. Such findings help one get a better understanding of the disease but also set a platform for developing effective therapeutic interventions that would result in non-recurrence and the possibility of longer lives for people with lung cancer.
As research in the area evolves, promise may come from more personalized and targeted therapies attacking not just the cancer cells but also the dramatically changing landscape of the microenvironment surrounding them in the treatment of lung cancer. Success in this respect can be achieved not merely by destroying cancerous cells but by disarming the very environment that protects those cells from treatments.