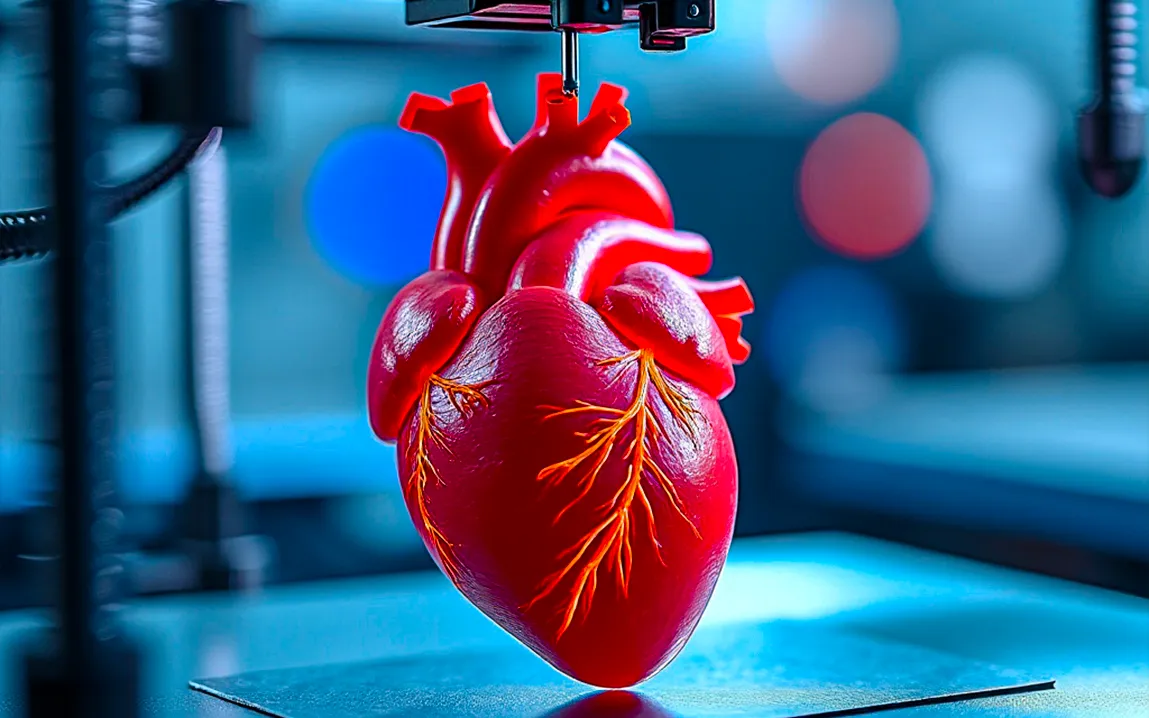
Over the last ten years, bioprinting has seen phenomenal growth in building functional human heart tissues. This could hold the key toward solving the acute shortage of donor organs and bringing a revolution to cardiovascular medicine.
The Evolution of Bioprinting
Bioprinting is an extension of traditional 3D printing wherein layer-by-layer assembly of biological materials is performed to construct complex tissue structures. It began in 1984 when the invention of stereolithography took place, and from that, other 3D printing technologies were possible. By 1988, scientists had already managed to adapt inkjet printers to deposit cells and were thus doing bioprinting. The late 1990s and early 2000s saw significant milestones, including the printing of an artificial scaffold for a human bladder in 1999 and a miniature functional kidney in 2002. These early achievements demonstrated the potential of bioprinting in regenerative medicine.
Breakthroughs in Heart Tissue Bioprinting
Bioprinting functional heart tissue has been the most challenging owing to the complex nature of the organ and the requirement for synchronized contractions. However, over the last couple of decades, scientists have been inching closer to realizing this quest. In 2019, a team of researchers from Israel successfully bioprinted a rabbit-sized heart, complete with blood vessels that could actually contract just like natural tissues. This was a leap forward and really demonstrated how it’s possible to bioprint anatomically correct and functional heart tissues.
Techniques and Innovations
The following bioprinting techniques have contributed significantly to these advancements:
- Sacrificial Writing into Functional Tissue (SWIFT): In this technique, living cells are densely packed, similar to those in real tissue; it carves out tunnels that can then be used as blood vessels to provide vital nutrients and oxygen. This SWIFT method effectively marries cell density with vascularization-a major barrier to the engineering of tissues.
- Stereolithographic (SLA) 3D Bioprinting: With controlled light or lasers, SLA bioprinting creates very accurate patterns in 2D and then lays them out to build 3D structures. This technique allows for creating complex shapes with high resolution of features, which is necessary for the exact recreation of the anatomy of the heart.
- Extrusion Bioprinting: This method is utilized in the continuous deposition of cell-laden bioinks, enabling it to fabricate 3D tissue models with high cellularity. This cell printing technique is well applicable for the fabrication of thick muscular walls of heart tissues.
Challenges and Future Directions
In spite of these improvements, a host of challenges now exist:
- Vascularization: The network of blood vessels within the heart has to be reproduced for more adequate viable tissue. Printing techniques like that of SWIFT show promise for improving vascular integration; however, there is some optimization, so this will be improved with larger-size tissues.
- Functional integration: Bioprinted cardiac tissues must achieve proper integration of current physiological tissues and well-coordinated contractility for effective clinical applications in therapeutic use.
- Regulatory and Ethical Considerations: As in the case of bioprinted tissues near clinical applications, these call for defined regulatory frameworks in addition to dealing with ethical considerations to guide studies and applications effectively.
Impact on Medicine
Bioprinting functional heart tissues has two important implications:
- Transplant: Bioprinted cardiac tissues can provide personalized solutions, ensuring supply when there is an acute demand due to an inadequate supply by donors.
- Drug Testing: Engineered heart tissues provide a platform for the testing of pharmaceutical compounds, thereby enhancing efficiency in drug development with reduced reliance on animal models.
- Disease Modeling: Patient-specific heart tissues can model cardiovascular diseases, thus enabling personalized medicine approaches and a better understanding of the mechanisms behind the disease.
Conclusion
Bioprinting functional human heart tissue has been achieved through a fusion of engineering, biology, and medicine. The challenges are formidable, but as much as has been accomplished so far, there is still a strong foundation for further progress to be made. Thus, as research continues to advance, this dream of bioprinted, fully functional human hearts takes one step closer to reality and will end up revolutionizing heart disease treatments and significantly improving the lives of many individuals.