Parkinson’s disease has been a problem for scientists and doctors for many years. It is a neurodegenerative disorder characterized by a set of symptoms including tremors, stiffness, and problems with mobility. This disease is due to the progressive loss of neurons that generate dopamine in the brain. Although therapies directed at replacing dopamine temporarily alleviate symptoms, they do not cure the root cause of neuronal degeneration. A promising new direction in drug design now seems to be emerging based on groundbreaking research into the structure of a receptor called GPR6. Elucidation of how this receptor works may open up completely new therapeutic avenues for Parkinson’s disease, possibly offering treatments that do not depend on the replacement of dopamine and thereby decrease associated side effects.
The Role of GPR6 in Parkinson’s Disease
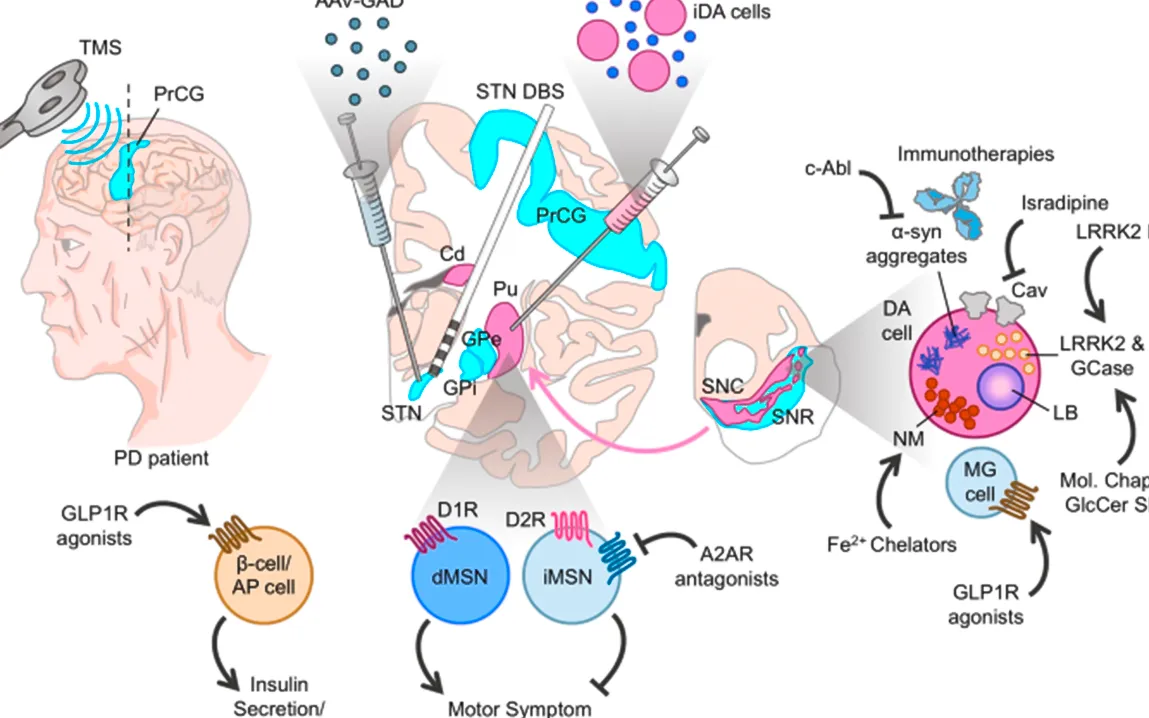
The receptor in question, GPR6, is a member of the G protein-coupled receptor family that plays an important role in the brain pathways controlling movement. More precisely, GPR6 is highly expressed in the striatum, especially within the striatopallidal pathway. This pathway is one of the key areas affected by Parkinson’s disease, in which the loss of dopamine-producing neurons disrupts the balance of signals needed for smooth, coordinated movement.
It has been demonstrated that even in the absence of an activating signal, GPR6 is active-a state described as “high basal activity.” This high level of activity can contribute to the dysfunctions in movement associated with Parkinson’s disease. The rationale for targeting GPR6 is that, rather than directly restoring dopamine levels, modulation of its activity provides a new avenue for treatments of some of the motor symptoms of Parkinson’s disease that avoids the adverse effects associated with current treatments, such as dyskinesia-the involuntary movements caused by long-term dopamine therapy.
Recent Studies
Recent research into the molecular structure of GPR6 has shed light on its function and how it can be targeted for therapeutic purposes. A team of scientists, led by Dr. Mahta Barekatain from the University of Southern California, used advanced techniques like mass spectrometry, mutagenesis, and computer modeling to explore the receptor’s structure in unprecedented detail. This finally came when they successfully captured the crystal structures of GPR6 in two key states-namely, without any ligand, a so-called “pseudo-apo” state, and in complex with inverse agonists, which are compounds that suppress its excessive activity.
One of the inverse agonists in the study, CVN424, has already shown promise in clinical trials; it improves motor symptoms in patients with Parkinson’s. CVN424 works by damping the overactive signaling caused by GPR6 and thus could provide a non-dopaminergic option for the treatment of this disorder. This is exciting because a method to treat Parkinson’s disease without exacerbating some of the negative side effects seen in the dopamine-based therapies, including motor fluctuations or involuntary movements, may be provided.
A New Paradigm in Drug Design
The importance of this discovery is in the paradigm shift it constitutes with respect to the treatment that could be given to people affected by Parkinson’s disease in the future. For decades, treatment strategies have focused mainly on restoring dopamine levels through drugs, usually levodopa. While these medications can alleviate symptoms, they cannot halt the underlying neurodegenerative process, nor do they address the abnormal signaling in areas such as the striatopallidal pathway that occurs as a result of neuron loss.
The new research into GPR6 provides a molecular blueprint for developing drugs that can target this specific receptor. Rather than simply boosting dopamine, drugs that modulate GPR6 activity could potentially rebalance the motor functions in Parkinson’s patients. This approach could be particularly indicated for treating the motor symptoms of the disease without the risk of triggering unwanted side effects, such as dyskinesia, commonly seen in patients who have been on dopamine therapies for long periods.
Future Perspectives on Parkinson’s Disease Treatment
The future in design thus has the potential to create a sea change in strategies toward Parkinson’s disease management. Currently, there is no cure for the disease; treatments only mitigate its symptoms. However, with increasing elucidation of such receptors like GPR6, possibilities abound for much more focused therapy that might even impede disease progression.
The implications of this research go beyond just GPR6. Success in understanding the structure of this particular receptor opens new avenues toward studying other GPCRs involved in Parkinson’s and other neurodegenerative diseases. In the case of GPR6, the hope is that future therapies will be both more selective and more effective, offering patients a better quality of life with fewer side effects.
Most of all, this discovery may yield a new class of drugs for use early in the course of the disease, maybe even before significant neuron loss sets in. This could mean that the management of the disease would be revolutionized: instead of being confined by devastating motor impairments, sufferers would be able to cope with the disease for far longer.
The Way Forward
Although studies of GPR6 have given promising results, the road to new, effective therapies is far from complete. Researchers will have to continue refining their understanding of how this receptor functions and interacts with other signaling pathways in the brain. In addition, while inverse agonists such as CVN424 show promise, further clinical trials are needed to confirm efficacy and safety in larger, more diverse patient populations.
Besides, much lies ahead in the development of drugs that precisely target GPR6 without affecting other receptors in the brain. The brain is a very complicated organ with a network of many signaling pathways, and reaching a perfect balance of activity in specific regions has been a major obstacle in the development of drugs targeting this organ.
However, the recent discoveries involving GPR6 give hope that a new generation of Parkinson’s treatments may be close at hand. For patients, this could mean therapies that are not only more effective but also with fewer side effects. If these new treatments become commonplace, they could mark an important step forward in the management of Parkinson’s disease, offering a better quality of life for patients and their families.
The excitement with GPR6 and other similar discoveries is yet another turning point in the fight against Parkinson’s disease. While much work is yet to be done, the future of therapeutics in Parkinson’s disease is brighter now than ever, driven by leaps in molecular biology and receptor-targeted drug design.