In a world increasingly bedeviled by antibiotic-resistant infections, a new discovery raises an alarm about the mechanisms that allow bacteria to bypass our best defenses. Researchers have found the important process through which foreign DNA, often carrying antibiotic resistance traits, “sneaks” past bacterial defenses. This breakthrough points out how bacteria can evolve to become resistant to antibiotics, further complicating treatment strategies and fuelling concerns about a public health crisis that could rival the worst pandemics in history.
The Rise of Antibiotic Resistance
Resistance to antibiotics has increased worldwide. The bacteria resistance causes prolonged hospitalization and extended days of intensive care, that raises mortality rates. In return to the invention of new different antibiotics and ways of treatment, the bacteria managed to become surprisingly adaptable to environmental conditions. For that matter, this process, largely based on bacterial genetic flexibility, has made them grow and spread with a particular trait in resistance so swiftly.
This ability of resistance to treatment is often associated with a group of small, mobile genetic elements known as plasmids. These are pieces of DNA that carry genes responsible for resistance to antibiotics, free from the bacterial chromosome, and can thus move between different bacteria, even across species, promoting the rapid spread of resistance genes.
In a landmark study, researchers have now found how these plasmids transfer the resistance genes into the bacterial chromosome, thereby fixing the resistance trait in the genetic makeup of the bacteria and allowing it to persist even in the absence of the plasmid. The discovery has profound implications for our understanding of how antibiotic resistance spreads and how it might be curtailed.
The Mechanism Behind the ‘Sneak’ of Foreign DNA
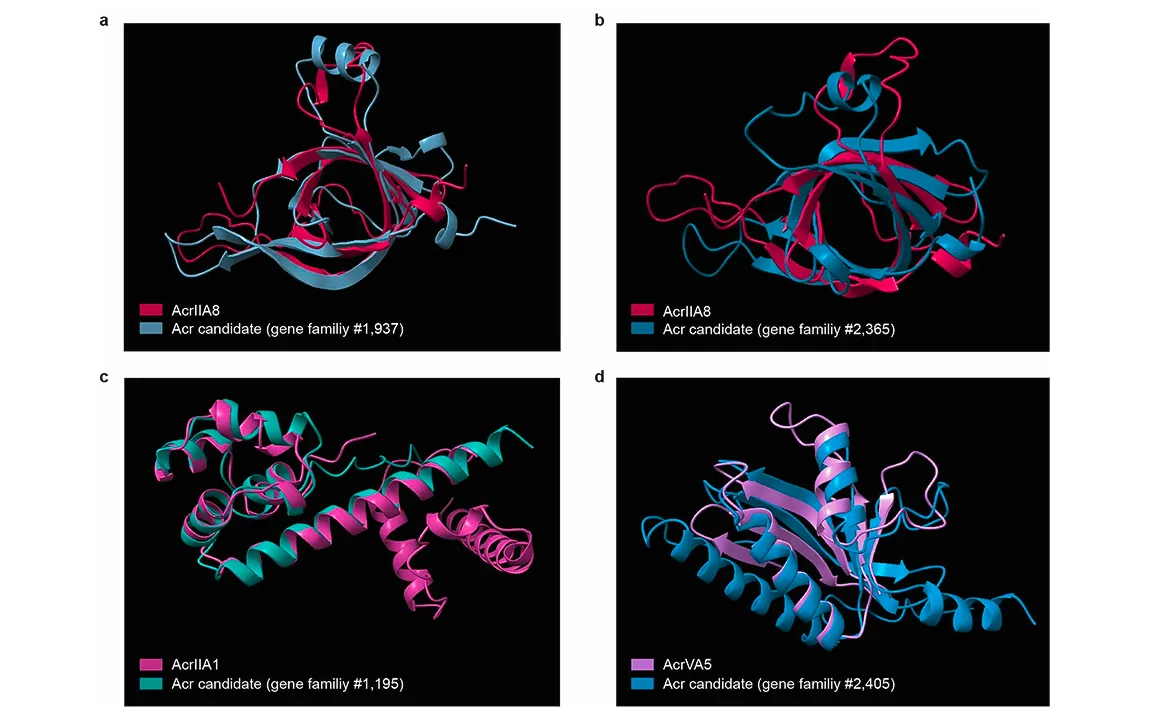
Probably one of the most important points of this research is the way bacteria are able to incorporate foreign DNA into their genomes through a process known as horizontal gene transfer. Traditionally, HGT was considered to occur mainly via plasmids, but new studies have shown that bacteria can also capture pieces of foreign DNA from the environment and integrate them directly into their chromosomes. This process allows bacteria to gain new traits, such as antibiotic resistance, without necessarily having to replicate the plasmid itself.
The cell membranes of bacteria are generally protected by barriers against the entry of foreign DNA. However, under certain conditions, they can “open up” their defenses and allow DNA from the outside world to enter. This can be done through naturally occurring transformations or through stress-induced mechanisms that make the bacteria more receptive to foreign DNA.
In the context of antibiotic resistance, this means that bacteria, which originally do not carry genes encoding antibiotic resistance, are able to integrate these into their genome. This way, they could survive the effect of antibiotics and pass on these resistance traits to their offspring, continuing the resistance cycle. This is one of the major reasons we are seeing more and more strains of bacteria that are resistant to multiple types of antibiotics, complicating treatment options and increasing the danger from infections.
The Role of Mobile Genetic Elements
Of particular interest is the horizontal process, a part of “jumping genes,” small mobile elements inside the bacterial genome; they allow it to jump from one place to another inside the genome, thereby facilitating its spreading resistance attributes. Indeed, studies have shown that these jumping genes migrate between bacterial populations, even across diverse environments. Thus, it has been able to achieve an unhindered spread through antibiotic resistance, even in non-related bacteria.
It points to the complexity of the problem of antibiotic resistance in that these mobile elements of genes can easily disseminate the resistance genes. It used to be confined to just a few genetically related bacteria, but it has since emerged into the world as one that may no longer be contained and could be transmitted with these jumping genes among bacteria across long distances and in diverse environments such as hospitals, farms, and even nature.
The Consequences for Public Health
Such findings have profound implications. One of the leading causes of death in the world is already antibiotic resistance, so this finding only increases the magnitude of the problem by finding that foreign DNA can more easily integrate into bacterial genomes. While horizontal gene transfer gives these bacteria resistance traits, making them more difficult to treat, this may result in longer hospital stays, complicated treatments, and increased risks of mortality.
Of particular concern is the emergence of so-called “superbugs”-bacteria resistant to multiple antibiotics-which creates a potentially serious public health threat. These bacteria are hard to keep under control with the current medications, and as they spread, they make infections harder to treat. If left to continue, antibiotic-resistant bacteria could render many of our current drugs ineffective, leaving us vulnerable to infections that were once easily treatable.
However, it is not within the confines of a hospital or clinical setting that this spread has been contained. The overuse of antibiotics in agriculture, especially in animal husbandry, has turned out to be another main driver of antibiotic resistance. Bacteria surviving in these milieus can then exchange their resistant genes with other bacteria and perhaps trigger an outbreak of resistant infections among humans.
Call to Action
Given the alarming nature of these findings, experts are calling for immediate action in the war against antibiotic resistance, including strict regulations on the use of antibiotics, increased investment in the development of new antibiotics, and greater efforts to monitor the spread of resistance genes both in healthcare and agricultural settings.
Another direction is basic research into the very ways bacteria acquire resistance. The elucidation of mechanisms by which bacteria “sneak” foreign DNAs into their genomes could help develop strategies to block such processes and, by doing so, make it more difficult for resistances to spread. In addition to traditional antibiotics, other options include bacteriophage therapy or vaccines, all currently under study for potential solutions to this increasing crisis.
Conclusion
The finding that foreign DNA can “sneak” past bacterial defenses to aid in the development of antibiotic resistance underlines the complexity and urgency of the antibiotic resistance crisis. As bacteria continue to evolve at an increasingly rapid pace, the need for new strategies to prevent the spread of resistance becomes ever more pressing. Researchers and public health officials must work together to better understand these mechanisms and develop effective solutions before antibiotic resistance becomes insurmountable.