A newly conducted study has opened up a whole new frontier as far as allergies and asthma are concerned by studying unique fungi inhabiting our nostrils. Researchers have now found that allergic rhinitis and asthmatic patients harbor unique fungal communities in their nose, which may have implications for our understanding of the diseases. The discovery provides a new insight into the triangle relationship that exists between our immune system, the environment, and the microorganisms that share our body space, while raising many more questions if fungi are causal agents or passengers in such common respiratory conditions.
The Fungal Communities in Our Noses
Every time we breathe in, we inhale not just air, but thousands of microscopic particles, including fungal spores. It is no secret that fungi are omnipresent in the environment. In fact, studies estimate that during certain seasons, more than 50,000 fungal spores per cubic meter of air can be present in the atmosphere. While most of these spores pass harmlessly through our respiratory system, some find a permanent residence in the nasal cavity. These fungal populations form what scientists call the “nasal mycobiome”-the community of fungi living inside our noses.
While for many years the focus of research into allergy and asthma has been on bacteria and other pathogens, fungi have all but been ignored. Recently, though, that’s starting to change. Fungi are now being recognized as an important part of our nasal microbiota, modulating immune responses and potentially contributing to conditions such as allergic rhinitis and asthma. One such study, published in *Frontiers in Microbiology* in December, provides the first evidence of significant differences in the nasal mycobiomes of individuals with and without these conditions.
Allergies and Asthma: How Fungi Might Be Involved
Allergic rhinitis, commonly known as hay fever, and asthma are both immune responses triggered by allergens like pollen, dust, or pet dander. These conditions affect millions of people worldwide, and their prevalence has been rising in recent decades. While we know that allergens cause an immune system overreaction in allergic individuals, the role of fungi in this process has remained unclear until now.
The study showed that allergic rhinitis and asthma patients had significantly different fungal communities in their noses compared to healthy individuals. More precisely, seven to ten of the most abundant fungal genera were different between the groups. This suggests that the types of fungi present in the nasal passages might be linked to the development or exacerbation of these conditions.
These results should not be over-interpreted, however, and the authors, led by Luis Delgado, are cautious: whereas the fungal composition in the nasal microbiome is apparently different between people suffering and not suffering from allergies, for example, it is not yet justified to state that fungi are the direct causes of these conditions. As Delgado said, “Causal relation may not be inferred with our study design and results.” In other words, the fungi might not be the root cause of allergic rhinitis or asthma but could instead be a byproduct of the inflammatory processes that go on in those conditions.
A Complex Relationship: Fungi, Immunity, and the Environment
The nasal cavity forms a very important first line of defense against environmental pollutants, bacteria, and viruses entering the body. It acts with a vigorous immune system as its defense mechanism that differentiates between harmful invaders and mere particles. Sometimes, in allergic individuals, this mechanism can overreact. Such an overreaction causes inflammation along with the typical symptoms associated with allergic rhinitis—sneezing, runny nose, congestion—or the more serious airway constriction seen in asthma.
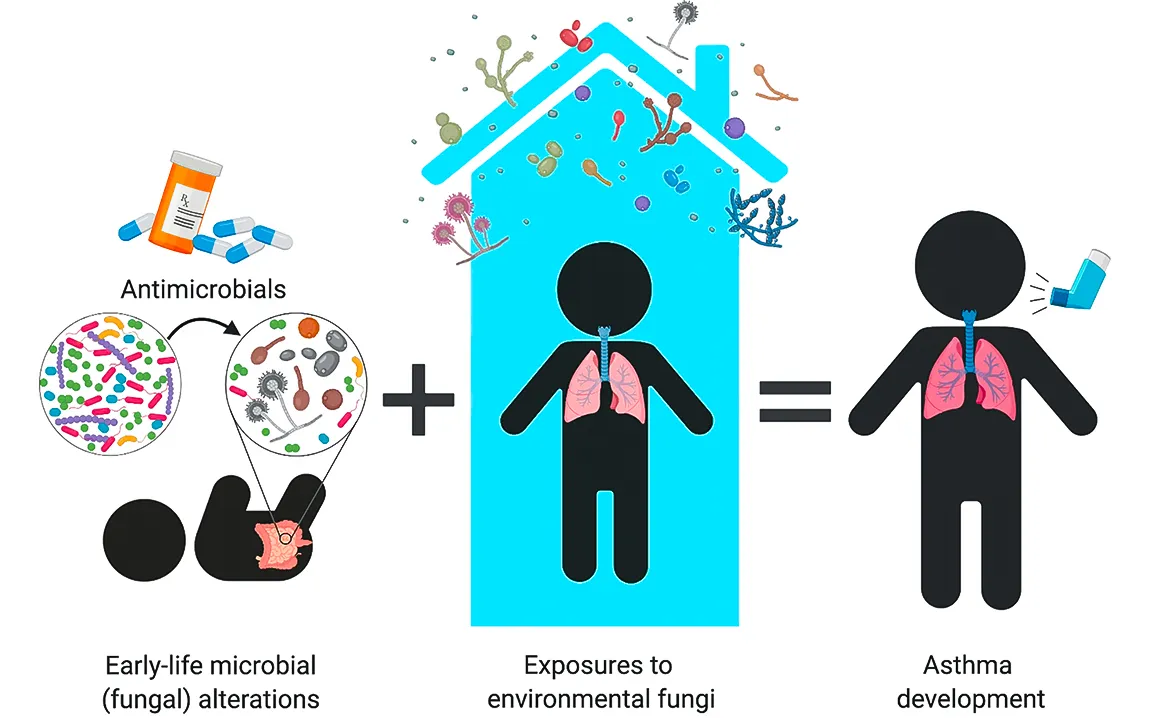
Fungi, along with bacteria and viruses, interact with this immune system regularly. Researchers have long known that exposure to a wide variety of microorganisms early in life can help “train” the immune system, making it less likely to develop allergic diseases. This has sometimes been called the “farm effect,” in which children raised on farms-naturally exposed to a diversity of microbes-are less likely to develop asthma or allergies. But what part fungi might play in this process has been poorly understood.
The surprising thing, though, is that the new study’s findings suggest the type of fungi present in the nasal passages may influence the immune response. Allergic rhinitis and asthma were characterized by a more diversified and complex network of fungal interactions than their negative counterparts. The mycobiome network was the richest in subjects suffering from both rhinitis and asthma, with several positive and negative interactions between different fungal species. In contrast, healthy individuals and those with rhinitis alone showed fewer and more positive interactions among fungi, reflecting a more balanced and less inflammatory immune response.
Future Research: Fungal Interactions and Disease
These findings are exciting because they offer a potential new avenue for understanding the underlying mechanisms of asthma and allergies. Although the role of fungi in these conditions is still speculative, the differences in fungal communities may reflect wider changes in the immune system. For example, the richness and complexity of the fungal network in patients suffering from both rhinitis and asthma may point toward a more aggressive immune response, or this may be due to the long-standing inflammation.
Furthermore, this study brings forward key questions regarding the interaction of bacteria and fungi within the nasal cavity. Although this present study only concerned fungi, the authors did indicate that bacteria more than likely have some part in this. Interaction of bacteria and fungi in the upper airways might hold the key to the general health of the respiratory microbiome. In some instances, the presence of certain bacteria may serve to augment the inflammatory effect of fungi, or vice versa.
Conclusion: A New Frontier in Allergy and Asthma Research
As studies of the nasal microbiome continue, investigation into the role of fungi in allergic diseases such as rhinitis and asthma is now taking on increased prominence. While it is too early to tell if fungi are a cause or a consequence of these conditions, the results of this study suggest that the fungi living in our noses are more important than we have given them credit for. The next steps in research will involve unraveling the complex interactions between fungi, bacteria, and the immune system. This will also help us to understand why some people are more susceptible to allergies and asthma but also pave the way for new therapeutic strategies that target the nasal microbiome to treat such chronic conditions.
In the future, as we learn more about this hidden world of nasal fungi, we may find that the key to treating allergies and asthma is not just medication, but in altering microbial communities that reside in our respiratory system. It might be the starting point that will usher in a new era in respiratory health-from symptoms-oriented to one of root cause treatment of the microbial imbalance causing chronic inflammation and disease.