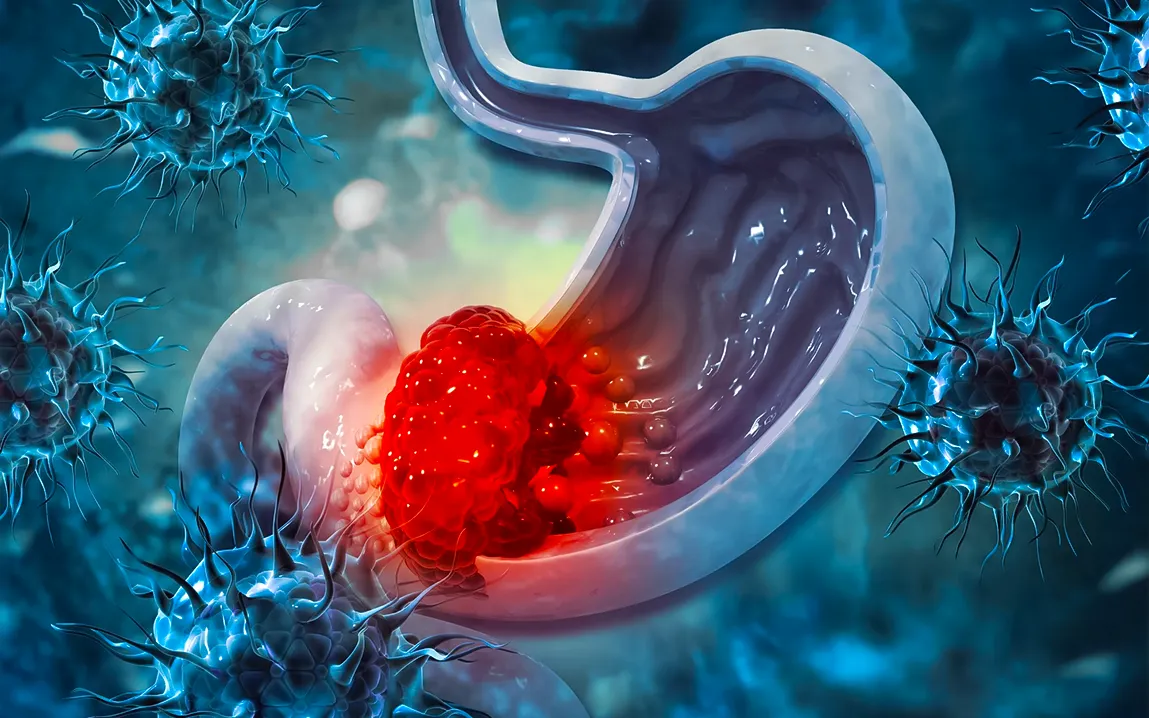
Stomach cancer, also called gastric cancer, is very serious because it often doesn’t cause any symptoms in the beginning. This means it’s usually found later, when treating it is harder and chances of survival are lower. One thing many people don’t know is that a common bacteria called Helicobacter pylori (H. pylori) can lead to stomach cancer. This bacteria affects more than half of the world’s population. Even though it’s so common, checking for this bacteria and its risks is still difficult and not done enough in medical care.
What is Helicobacter pylori?
Pylori is a bacterium that lives in the acidity of the stomach. Because it is spiral-shaped, it burrows into the lining of the stomach so the body’s defense systems cannot destroy it. So common is this bacterium that more than half the world’s population harbors it, although most infected individuals remain asymptomatic. In fact, some studies put the infection rate as high as 80% of the population in developing countries, although the percentage is much lower in developed countries due to better hygiene and healthcare standards.
In most individuals, an H. pylori infection is not serious. For others, when left untreated for extended periods of time, it can result in serious health issues such as chronic gastritis, peptic ulcers, and stomach cancer.
The Connection Between H. pylori and Stomach Cancer
The association of H. pylori with stomach cancer had been realized since the early 1980s when the Australian scientists Barry Marshall and Robin Warren discovered the role of the bacterium in causing gastritis and ulcers. Over time, research has shown that persistent infection with H. pylori leads to chronic inflammation of the stomach lining. This ongoing irritation and damage increase the likelihood that cells in the stomach lining will undergo mutations, eventually leading to cancer.
All strains of H. pylori are not equally virulent. Certain strains produce a particular toxin known as CagA (cytotoxin-associated gene A), which plays a critical role in the development of stomach cancer. This toxin impairs the normal function of the cells of the stomach and favors abnormal cell growth. Individuals infected with CagA-positive strains have a much greater risk of stomach cancer than those with other types of H. pylori infection.
This notwithstanding, H. pylori is linked with an increased risk of a variety of other stomach diseases, which include gastric lymphoma, the type of immune system malignancy affecting specific cells that reside in the stomach’s lining. For such kinds of cancers, an estimation of very significant reduction may be anticipated after early H. pylori eradication; these observations enhance the rationale to detect the infection and administer appropriate therapy.
Problem with Screening and Diagnosis
While the link between H. pylori and stomach cancer is established, diagnosing the infection and its long-term effects is anything but straightforward. H. pylori infections often do not exhibit overt symptoms, and when they do, they are frequently confused with other gastrointestinal disorders, such as indigestion or heartburn. Not everyone infected with H. pylori will go on to develop stomach cancer. The presence of specific bacterial strains, genetic predispositions, lifestyle factors, and environmental influences are all contributory factors that can decide whether an infection leads to cancer.
The tests to detect the infection of H. pylori are mainly available in the forms of blood tests, stool tests, breath tests, and endoscopic biopsies. Most of these types of tests are not really universally available, especially to poor settings. And usually, when available, they often rely on symptomatic or even those who have known risk factors for gastric cancer, like a history of gastric cancer in the first-degree relative or ulcers.
One of the big problems with mass screening for H. pylori is that most people harboring the bacterium have no symptoms and may never go on to develop stomach cancer. This puts physicians in a bind: while finding and eliminating the bacterium in at-risk individuals might reduce cancer incidence, doing so in a blanket fashion could result in unnecessary treatments and a rise in antibiotic resistance. Furthermore, there has been no uniform guideline to date concerning who should or should not be tested, let alone treated, for the disorder.
Indeed, where there is a high incidence of infection, as in parts of Asia and South America, stomach cancer also tends to be very prevalent. In such regions, selected screening and treatment of H. pylori infection have been demonstrated to reduce gastric cancer incidence quite significantly. Even so, even in these areas, the logistics of screening large populations can be daunting, while the costs of mass treatment may be prohibitive.
Prevention and Treatment: Is There Hope?
Although it’s hard to find stomach cancer early, treating H. pylori infections can help prevent it. Antibiotics can get rid of the bacteria in the stomach, and this has been shown to greatly lower the chance of getting stomach cancer, especially if the treatment happens early. Research shows that getting rid of H. pylori can reduce the number of stomach cancer cases by up to 50% in some groups of people.
For those already diagnosed, the course of treatment ranges based on the stage and place the cancer is found. In the earliest stages, stomach cancer is normally able to be treated through surgery, but advanced cases can include chemotherapy, radiation, or combined treatments. Advanced stomach cancer has relatively low survival rates, and prevention remains a very vital strategy.
Lifestyle modifications also have a role in the prevention of stomach cancer. Avoidance of smoking, limitation of alcohol intake, and limitation of salty and processed foods can decrease the risk of stomach cancer. Some studies indicate that an increased intake of fruits and vegetables, rich in antioxidants, may reduce the risk of cancer, though this is still under research.
The Global Perspective
The finding that H. pylori is a leading cause of stomach cancer is a big step forward in understanding this serious illness. However, solving the worldwide problem of this infection involves more than just medical expertise. Public health efforts that encourage better hygiene and sanitation are crucial for slowing the spread of the bacteria, particularly in poorer countries. Additionally, creating vaccines to stop H. pylori infections could be very helpful, although these vaccines are still being studied.
The fight is far from over, as stomach cancer and H. pylori infection remain; however, this continued emphasis on early detection, treatment, and prevention might turn the tide toward improved population health. Someday, with increased awareness and trying to meet the challenges in screening and treatment, the world might see a decrease in not only H. pylori infection rates but also in the incidence of stomach cancer.
Moving forward, the difficult balance must be struck among the three competing interests of needs for universal screening and treatment versus realities of cost, access, and antibiotic resistance. One can hope that the targeting of such efforts means that fewer victims will be suffering the tragedy of this cancer of the stomach caused by a ubiquitous bacterium and largely preventable.