Recent breakthroughs in Alzheimer’s disease research have led to new revelations concerning the development of the neurodegenerative ailment. It has chiefly been determined how tau filaments-the hallmark protein linked to Alzheimer’s disease-are related to some of the extracellular vesicles that mediate the communication of neurons in the brain. This emerging research illustrates how tau propagates in a brain and causes defects in cognition in the affected individuals.
Tau and Its Role in Alzheimer’s Disease
Tau is a protein that plays a major role in naturally supporting and stabilizing microtubules of neuronal cells. However, if it becomes abnormally phosphorylated-which occurs in Alzheimer’s disease and other tauopathies-and it forms twisted tangles inside neurons. These tau tangles have been described as one of the identifying pathological characteristics of Alzheimer’s, believed to result in the malfunction and subsequent death of neurons.
Tau is toxic in both the cell where it first gathers and spreads to nearby cells, leading to increasingly negative impacts on the progress of the disease. Its way of spreading from a single cell to another is peculiar because toxic tau moves through small extracellular vesicles; basically, it’s a bunch of tiny, membrane-wrapped pieces released by cells. Indeed, these vesicles, usually employed by cells as little shuttles transporting proteins, lipids, or other molecules, provide various means for intercellular communication. However, in the case of Alzheimer’s, these vesicles may carry harmful tau aggregates, allowing them to spread across the brain.
The Groundbreaking Study
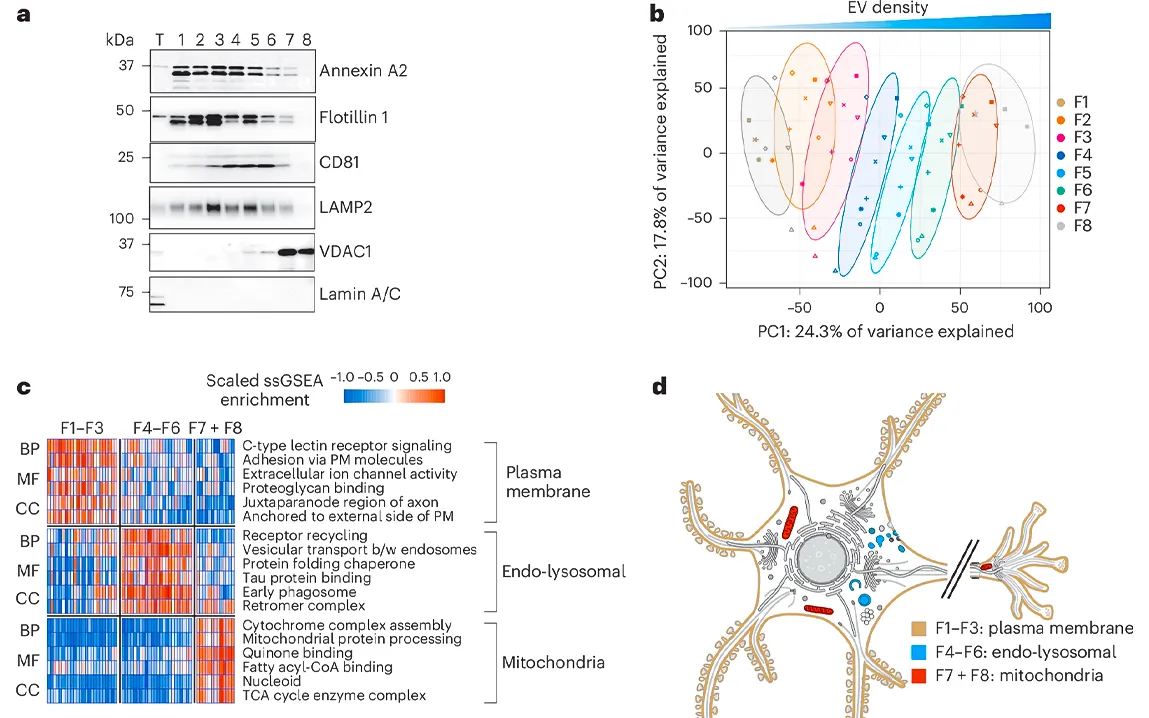
One of the most important studies in recent times has discovered new details about how tau filaments are associated with extracellular vesicles in Alzheimer’s disease. The research team, led by experts from the UK Dementia Research Institute and the MRC Laboratory of Molecular Biology used a combination of advanced techniques, including cryo-electron tomography (cryo-ET) and mass spectrometry, to analyze brain tissue from Alzheimer’s patients. Their work revealed one striking finding: tau filaments, in their amyloid form, were tethered to the membranes of extracellular vesicles within the brain.
The study showed that these vesicles were enriched with tau filaments, especially those resembling the paired helical filaments characteristic of Alzheimer’s disease. Moreover, the authors found that tau in these vesicles was not free but instead anchored to the vesicle membrane, providing a new perspective on how tau aggregates are trafficked in the brain. This finding points to the implication that tau fragments may be selectively packaged into vesicles, rendering them more stable and capable of spreading into neighboring cells.
How Do Extracellular Vesicles Contribute to Tau Propagation?
Extracellular vesicles constitute a heterogeneous family of material shed from a large number of brain cells, consisting mainly of neuronal and glial cells and responsible for a multitude of physiological processes, including cell communication and waste disposal. However, in Alzheimer’s, they seem to play a much darker role. The study suggests that when tau protein aggregates become too big or misshapen for normal cell-mediated degradation, they might instead be packaged into extracellular vesicles.
Once the vesicles leave the cells, they can be taken up by other neurons or glial cells and potentially spread the toxic tau to new brain regions. This could account for the progressive nature of tau pathology in Alzheimer’s, whereby the disease spreads from one region of the brain to another. The researchers found a distinctive characteristic of the vesicles in which the tau was assembled: tau is tethered to the vesicle membrane, which can influence how the tau aggregates initially form and enter the vesicles.
The findings also showed that tau filaments in these vesicles were similar to those in neurofibrillary tangles within neurons, though in truncated forms. This could mean that tau in vesicles is an intermediate state, not fully mature or aggregated, yet still competent for cell-to-cell propagation of the pathology.
Implications for Early Diagnosis and Therapeutic Strategies
The fact that tau filaments are packaged into EVs opens new perspectives not only toward the early detection of the disease but also toward treatment. The presence of vesicles containing tau in fluids within the brain, including cerebrospinal fluid, provides a potential biomarker for early-stage Alzheimer’s that predates extensive neurodegeneration.
According to the therapeutic approach, mechanisms of tau transport and spread via extracellular vesicles could be targets for new treatments. Should scientists learn how to block the release or the uptake of these vesicles, it would be a further step toward repressing the passing of tau pathology throughout the brain-in accordance with the hopes of chronic patients. Additionally, knowledge of what specific proteins and structures are involved in the packaging of tau into vesicles could lead to the development of drugs that may help to arrest this phenomenon and thus take the whole course of the disease downstream from it.
Conclusion
The investigation into the correlation between tau filaments and extracellular vesicles is thus a landmark in the investigation of Alzheimer’s disease pathology. These provide a deeper insight not only into how tau spreads through the brain but also point toward new ways to detect and treat the disease. This would entail targeting the mechanisms that enable tau to be packaged into vesicles and therefore be spread to neighboring cells; such strategies may provide effective means of combating Alzheimer’s disease and offer hope to the millions of people who, across the world, have become victims of this appalling neurodegenerative disease. The next steps in research will likely focus on translating these findings into clinical applications, potentially changing the way we diagnose and treat Alzheimer’s in the near future.